Laparoscopic gynecologic surgeries are a revolutionary advancement in women's healthcare, providing minimally invasive solutions to complex medical conditions. By utilizing advanced laparoscopic techniques, these procedures offer shorter recovery times, reduced pain, and smaller scars compared to traditional open surgeries. This article explores the applications of laparoscopic surgeries for hysterectomy, endometriosis removal, ovarian cystectomy, and tubal ligation, delving into their procedures, benefits, and key considerations.
Minerva Health Solutions delivers top-quality medical equipment to support optimal patient outcomes. Browse our portfolio today for innovative solutions tailored to your needs.
What Are Laparoscopic Gynecologic Surgeries?
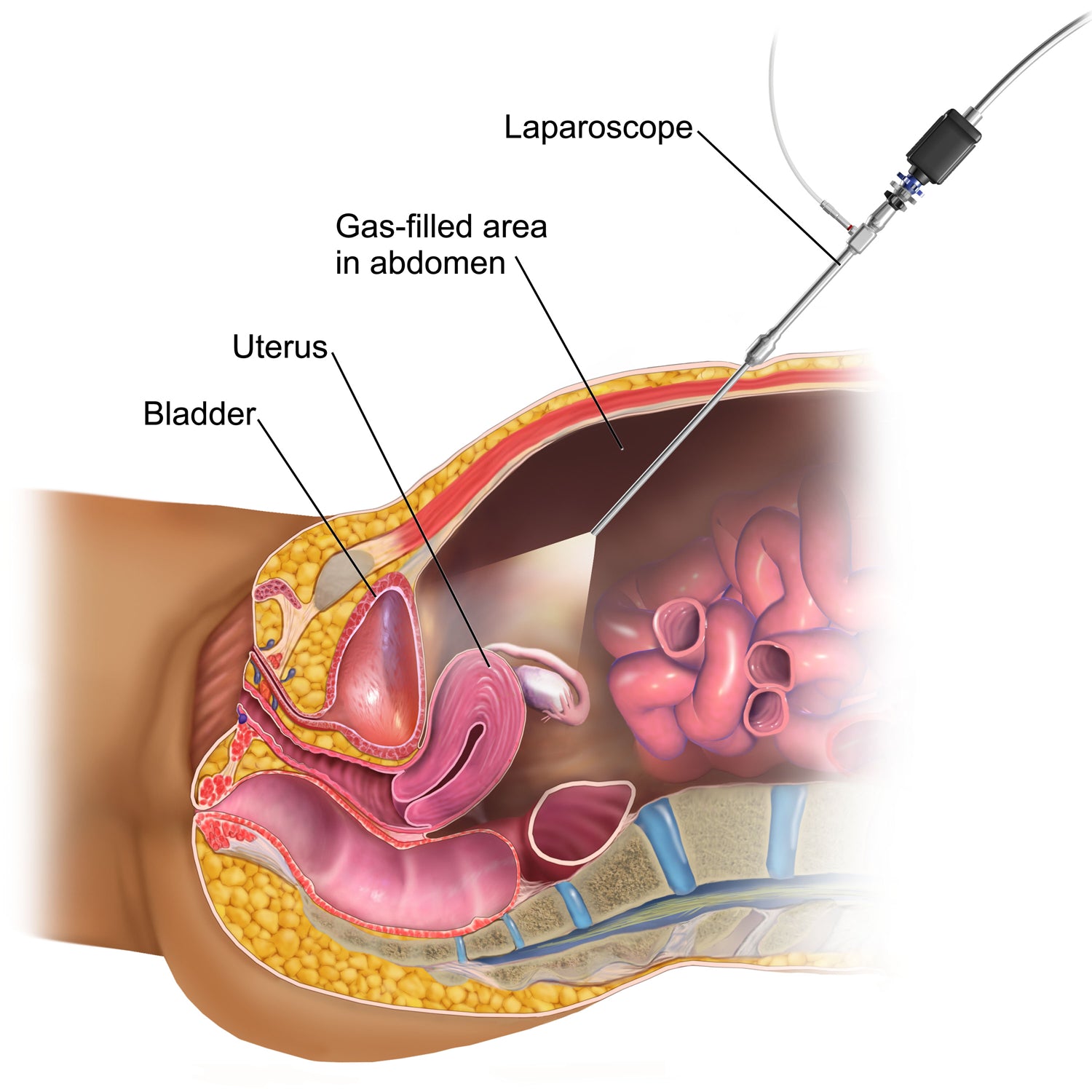
Laparoscopic gynecologic surgeries involve the use of a laparoscope—a thin tube equipped with a high-resolution camera and light—to perform intricate procedures through small incisions in the abdomen.
Key Benefits:
- Minimally invasive: Smaller incisions reduce trauma to the body.
- Faster recovery: Patients can resume daily activities sooner.
- Less postoperative pain: Compared to traditional open surgeries.
- Enhanced precision: Surgeons have better visualization of internal organs.
This approach is widely used for addressing reproductive health issues, providing a safer and more effective alternative for patients.
Applications of Laparoscopic Surgeries
-
Laparoscopic Hysterectomy
A hysterectomy, the surgical removal of the uterus, is often performed to treat conditions like:
- Fibroids
- Endometrial cancer
- Severe uterine bleeding
Procedure:
- Small incisions are made in the abdomen.
- The uterus is detached and removed using specialized laparoscopic instruments.
- Some cases may also involve the removal of ovaries or fallopian tubes.
Benefits:
- Lower risk of infection compared to open surgery.
- Reduced hospital stay, often less than 24 hours.
- Preserves abdominal muscles, leading to quicker recovery.
Key Considerations:
Patients should consult their doctor about hormonal implications, especially if ovaries are removed.
-
Endometriosis Removal
Endometriosis, a painful condition where tissue similar to the uterine lining grows outside the uterus, can lead to:
- Chronic pelvic pain
- Infertility
- Heavy menstrual bleeding
Role of Laparoscopy:
- Identifies and removes endometrial tissue growth.
- Minimizes damage to surrounding organs.
- Improves fertility outcomes in many patients.
Why Choose Laparoscopy?
- Accurate diagnosis and targeted treatment.
- Smaller incisions mean faster healing and less discomfort.
- Patients often experience significant pain relief and better quality of life following the procedure.
-
Ovarian Cystectomy
This procedure focuses on removing ovarian cysts while preserving healthy ovarian tissue, crucial for hormonal balance and fertility.
Common Types of Cysts:
- Functional cysts
- Dermoid cysts
- Endometriomas
Procedure Steps:
- A laparoscope is inserted through a small incision.
- The cyst is carefully removed, ensuring the ovary remains intact.
- Any potential adhesions are addressed.
Post-Surgery Recovery:
- Most patients return home the same day.
- Normal activities can usually resume within 1-2 weeks.
-
Tubal Ligation
Tubal ligation, often referred to as "getting your tubes tied," is a form of permanent contraception.
How It's Done:
Fallopian tubes are blocked, cut, or sealed using laparoscopic tools.
Prevents eggs from reaching the uterus for fertilization.
Benefits of the Laparoscopic Approach:
Minimal scarring.
Procedure takes less than an hour.
Highly effective and reliable contraception.
What’s Next?
In the second part of this article, we will discuss the advantages of laparoscopic techniques in depth, address risks and limitations, and offer tips for optimal recovery. Stay tuned to explore FAQs and actionable advice for patients considering these groundbreaking procedures.
Laparoscopic Gynecologic Surgeries: Recovery, Risks, and FAQs
Advantages of Laparoscopic Gynecologic Surgeries
Laparoscopic surgeries have revolutionized gynecological care by offering a minimally invasive alternative to traditional procedures. Patients benefit from quicker recovery and fewer complications. Here’s a closer look:
Key Benefits:
Shorter Recovery Time: Most patients resume normal activities within 1-2 weeks.
Minimal Scarring: Small incisions result in tiny, almost invisible scars.
Lower Infection Risk: Reduced exposure of internal organs lowers the chance of infections.
Enhanced Precision: High-definition cameras enable surgeons to work with greater accuracy.
Less Pain: Smaller incisions and minimal tissue disruption lead to reduced postoperative pain.
For patients, these benefits translate to a more comfortable experience with improved outcomes.
Potential Risks and Complications
While laparoscopic surgeries are generally safe, there are some risks to consider:
Bleeding: Though rare, internal bleeding can occur.
Infection: Proper wound care minimizes this risk.
Organ Damage: Accidental injury to nearby organs, such as the bladder or bowel, is a possibility.
Hernia Formation: Incision sites may develop hernias if not healed properly.
Anesthesia Reactions: Some patients may experience adverse effects from general anesthesia.
How to Mitigate Risks:
Choose a surgeon with extensive laparoscopic experience.
Follow pre- and post-surgical care instructions meticulously.
Discuss your complete medical history with your healthcare provider.
What to Expect During Recovery
Post-Surgery Care Tips:
Rest: Allow your body time to heal by avoiding strenuous activities for the first week.
Pain Management: Use prescribed painkillers or over-the-counter medications as directed.
Diet: Gradually resume a balanced diet. Start with light meals to avoid gastrointestinal distress.
Incision Care: Keep incision sites clean and dry to prevent infections.
Follow-Up Visits: Attend all scheduled appointments to ensure proper healing.
Typical Recovery Timeline:
First 24 Hours: Rest and limit physical activity.
1-2 Weeks: Resume light daily activities; avoid heavy lifting.
4 Weeks: Most patients return to full activity, including exercise.
Addressing Hormonal Impact
Laparoscopic procedures, especially those involving ovary removal, can significantly affect hormonal balance.
Key Considerations:
Hysterectomy with Oophorectomy: Removing ovaries leads to immediate menopause.
Hormone Replacement Therapy (HRT): Consider HRT to manage symptoms like hot flashes or mood swings.
Fertility Concerns: Patients planning future pregnancies should explore alternatives or fertility preservation methods before surgery.
It’s crucial to discuss these aspects with your gynecologist to make informed decisions.
Frequently Asked Questions (FAQs)
- How long does laparoscopic gynecologic surgery take?
Procedures typically last between 1-3 hours, depending on the complexity and the type of surgery.
- Will I need hospitalization?
Most laparoscopic surgeries are outpatient, meaning you can go home the same day. However, some complex procedures may require a short hospital stay.
- Can I have children after laparoscopic gynecologic surgery?
Hysterectomy: Removes the uterus, eliminating the possibility of pregnancy.
Endometriosis or Cystectomy: Fertility can improve post-surgery, depending on the condition treated.
- How soon can I return to work?
You can usually return to light work within 1-2 weeks, depending on your overall recovery.
- Are laparoscopic surgeries covered by insurance?
Most insurance plans cover these procedures, but it’s best to verify specifics with your provider.
Laparoscopic gynecologic surgeries offer state-of-the-art solutions for a wide range of conditions, from hysterectomy to ovarian cyst removal. With minimal invasiveness, faster recovery, and fewer complications, they represent the future of women’s healthcare. However, thorough consultation with a qualified surgeon is vital to ensure the best outcomes.
If you’re considering laparoscopic gynecologic surgery, prepare yourself with knowledge and choose a trusted healthcare provider to guide you through the journey.
Contact Minerva Health Solutions to learn more about our laparoscopic portfolio or to request a quote. Let us be your partner in advancing healthcare technology.