Benign anorectal disorders, such as chronic constipation and fecal incontinence, often stem from pelvic floor dysfunction. The 2021 ACG Clinical Guidelines underscore the transformative role of anorectal biofeedback therapy using balloon catheters—a non-invasive, evidence-based intervention that addresses these challenges head-on. Here’s how this therapy stands out, backed by clinical insights and outcomes.
Corrects Pelvic Floor Dyssynergia with Precision
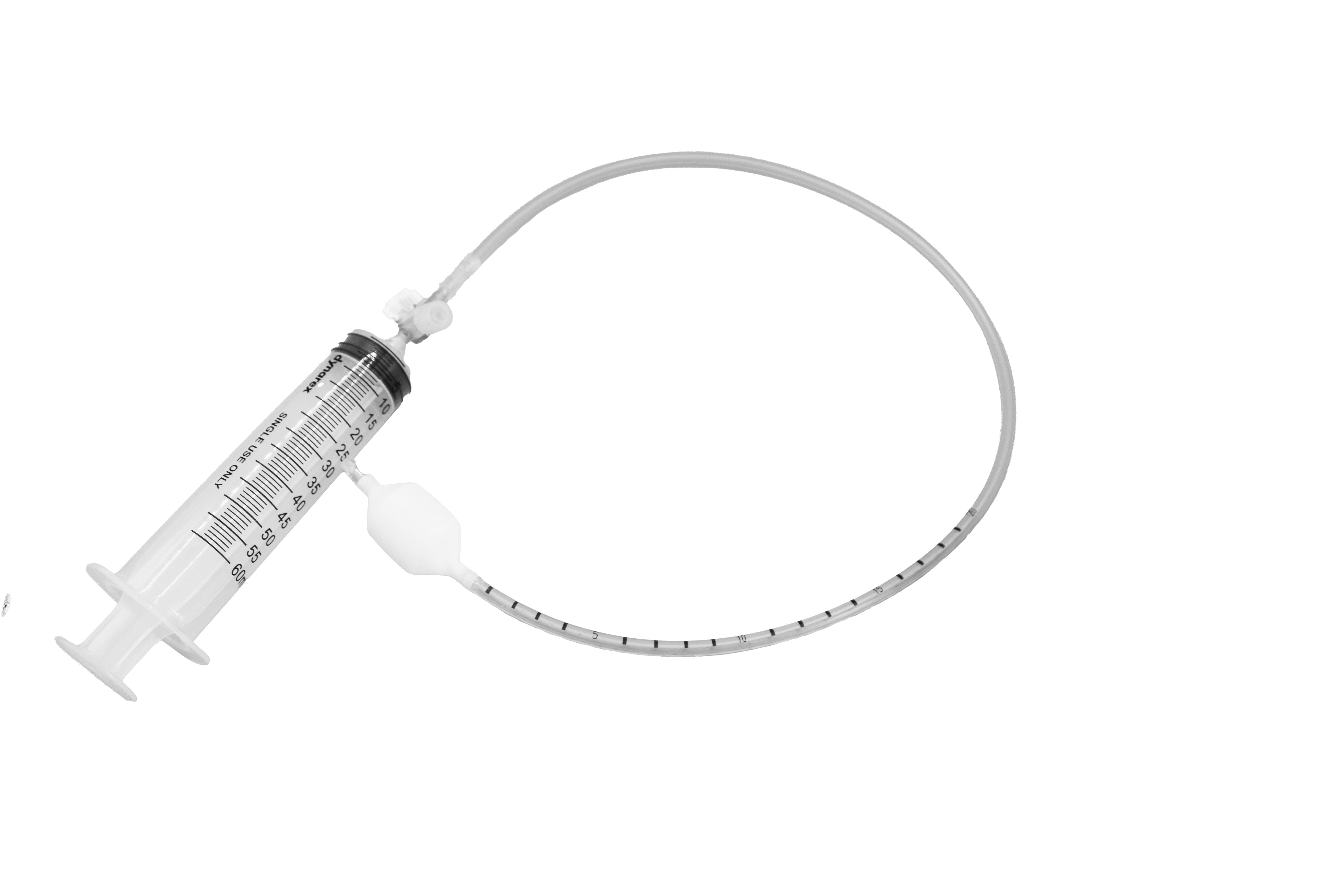
Biofeedback therapy employs real-time visual or auditory feedback from balloon catheters to retrain pelvic floor muscles. Patients learn to synchronize abdominal pressure with anal sphincter relaxation—a critical step for effective defecation.
- 79% of patients with dyssynergic defecation (paradoxical muscle contraction) achieve normalized muscle coordination after biofeedback, compared to minimal improvement in control groups1.
- This approach directly targets the root cause of evacuation disorders, unlike laxatives or fiber supplements that only alleviate symptoms temporarily.
Improves Rectal Sensitivity and Evacuation Efficiency
Balloon catheters recalibrate rectal sensory thresholds, addressing hypersensitivity or hyposensitivity that disrupts bowel urgency or completeness.
- Patients using biofeedback exhibit 16-second improvements in balloon expulsion times vs. 1-second gains in non-biofeedback groups.
- Enhanced sensory feedback helps patients recognize the urge to defecate, reducing episodes of incontinence or incomplete evacuation.
Non-Invasive Alternative to Surgery
For chronic constipation or fecal incontinence unresponsive to first-line treatments, biofeedback offers a low-risk solution.
- Avoids surgical complications (e.g., infection, prolonged recovery) and is strongly recommended in the ACG guidelines as a first-line therapy.
- Protocols are customizable: Balloon inflation volumes and training intensity can be adjusted to individual needs.
High Patient Satisfaction and Sustained Results
Clinical trials highlight strong patient-reported outcomes:
- 78% report partial or complete satisfaction, with reduced reliance on laxatives and fewer incontinence episodes.
- Benefits persist long-term, with 70–90% sustaining symptom relief years after completing therapy.
Dual Diagnostic and Therapeutic Utility
Balloon catheters serve a dual role:
- Diagnostic: Measures rectal pressure, compliance, and sensory thresholds via tests like the Balloon Expulsion Test (BET) and anorectal manometry.
- Therapeutic: The same device guides retraining, streamlining care from evaluation to treatment.
Who Benefits Most?
- Chronic constipation from pelvic floor dyssynergia.
- Fecal incontinence due to weakened sphincters or neuropathy.
- Post-surgical patients recovering from sphincter repairs or hemorrhoidectomies.
Anorectal biofeedback therapy with balloon catheters is a cornerstone of modern management for functional bowel disorders. By combining physiological retraining with patient-specific feedback, it offers a safe, effective, and durable solution—aligning with the ACG’s emphasis on evidence-based, personalized care. If conventional treatments fall short, this therapy warrants serious consideration in collaboration with a gastroenterologist or pelvic floor specialist.
Wald, A., Bharucha, A. E., Limketkai, B., Malcolm, A., Remes-Troche, J. M., Whitehead, W. E., & Zutshi, M. (2021). ACG Clinical Guidelines: Management of Benign Anorectal Disorders. American Journal of Gastroenterology, 116(10), 1987–2008. https://doi.org/10.14309/ajg.0000000000001507