Pelvic floor physical therapists are increasingly using anorectal balloon catheter training to treat chronic constipation, dyssynergic defecation, rectal pain, and fecal incontinence in a more targeted way. By combining controlled rectal distension with biofeedback, rectal balloon training goes beyond verbal cueing and basic pelvic floor exercises to provide task-specific retraining of bowel sensation and coordination.
Who this article is for
This article is written for pelvic floor physical therapists and pelvic health clinicians who are asking, “When should I actually use a rectal balloon, what does the evidence say, and what does a typical protocol look like?” You will find practical clinical indications, short evidence spotlights from randomized trials and guidelines, and protocol snapshots you can adapt in your own practice.
When and why to use anorectal balloon catheters
Many of your bowel patients already sound familiar: they strain for long periods, still feel incompletely emptied, or rush to the bathroom with very little warning. What is less obvious without specific testing is how much of that difficulty comes from impaired rectal sensation, disordered coordination of the abdominal wall and pelvic floor, or both. Anorectal balloon catheters give you a standardized way to explore those questions and then retrain more efficient patterns in a controlled, repeatable setting.
Key indications in pelvic floor physical therapy
Fecal incontinence and urgency
Patients with fecal incontinence often report minimal warning time, strong urgency, or leakage after obstetric injury, anal surgery, or pelvic radiation. In many of these cases, rectal hyposensitivity, reduced maximum tolerable rectal volume, or poor urge control can be just as important as sphincter strength. Balloon assessments let you quantify thresholds for first sensation, desire to defecate, and strong urge, and then train patients to recognize and manage those urges more effectively.
Chronic constipation and dyssynergic defecation
Chronic constipation with outlet dysfunction or dyssynergic defecation is common in pelvic health caseloads. Patients may describe prolonged straining, a feeling of blockage, or the need for digital maneuvers despite adequate stool consistency and fiber intake. Dyssynergic patterns such as paradoxical anal contraction or failure of pelvic floor relaxation during bearing down are frequently associated with impaired balloon expulsion. Rectal balloon training allows you to simulate defecation and practice coordinated abdominal pressurization with pelvic floor relaxation while directly observing and correcting faulty strategies.
Anismus and high-tone pelvic floor
Some patients can relax the pelvic floor voluntarily in exam positions but cannot “let go” when asked to defecate. In these cases, the defecatory act itself is the challenging task, not isolated relaxation drills. Balloon-assisted expulsion training provides graded exposure to the sensations and mechanics of emptying while reinforcing diaphragm-driven abdominal pressure and softening of the anal sphincter and pelvic floor.
Rectal pain and functional anorectal disorders
Patients with chronic proctalgia or non-specific rectal pain may benefit from controlled rectal distension combined with relaxation strategies. Through careful titration of inflation volumes and the use of breathing, imagery, and biofeedback, balloon work can help desensitize painful or fear-provoking sensations while restoring a sense of control over the defecatory process.
Rectal prolapse and internal intussusception
For patients with rectal prolapse or internal intussusception, whether managed conservatively or post-surgically, balloons allow you to practice urge management and coordinated emptying without repeated straining against stool. This can be especially helpful early in recovery, when heavy straining may be uncomfortable or discouraged.
Across these presentations, anorectal balloon catheters help clinicians move from generalized advice (“don’t strain,” “do your Kegels”) to individualized, objective training plans based on measurable sensory thresholds and task performance.
Evidence supporting rectal balloon biofeedback
The use of anorectal balloon catheters is not just an interesting niche; it is supported by randomized controlled trials and international guideline statements for benign anorectal disorders. For pelvic floor physical therapists, this evidence base positions rectal balloon biofeedback as a core tool rather than an experimental add-on.
Randomized trials in dyssynergic defecation and constipation
Randomized trials of biofeedback-based programs that include rectal balloon training have shown significant improvements in dyssynergia, constipation symptoms, and anorectal physiology compared with standard care or laxative therapy alone. In patients with dyssynergic defecation, biofeedback protocols that target both coordination and sensory function can normalize balloon expulsion in a substantial proportion of participants, improve colonic transit, and reduce reliance on laxatives. Follow-up data show that these improvements can persist for years, especially when patients continue home exercises that reinforce the learned defecation patterns.
Rectal balloon training in fecal incontinence
In fecal incontinence, adding rectal balloon training to pelvic floor muscle training appears to offer additional benefit over exercises alone. One randomized trial comparing pelvic floor muscle training with and without balloon-based sensory and urge training found that both groups improved incontinence scores, but the combined group achieved greater increases in maximum tolerable rectal volume and better self-reported urgency control and quality of life. For clinicians, this suggests that balloon work is most powerful when integrated into a comprehensive rehabilitation program rather than used as a stand-alone intervention.
Guideline-level recommendations
Consensus guidelines from major motility and gastroenterology societies endorse biofeedback therapy, often including rectal balloon and balloon expulsion components, as a first-line or strongly recommended option for defecatory disorders and selected cases of fecal incontinence. These guidelines emphasize that, when available, biofeedback should be prioritized ahead of repeated medication trials or more invasive procedures for patients with documented dyssynergia or outlet dysfunction. This aligns closely with the skill set of pelvic floor physical therapists who can deliver structured, skills-based training.
Practical rectal balloon training protocols
While exact parameters will vary by equipment, clinic setup, and patient tolerance, most rectal balloon training protocols share three core elements: sensory work, expulsion training, and urge or continence training, all layered onto a foundation of pelvic floor muscle training and biofeedback.
Sensory assessment and rectal sensory training
A typical session starts with sensory mapping. With the patient in left sidelying or supported hooklying, the catheter is inserted so the balloon rests just inside the rectum according to manufacturer guidance. The balloon is gradually inflated in small volume increments, often 10–20 mL at a time, while you ask the patient to report first sensation, desire to defecate, and strong urge. These values provide an objective baseline for rectal sensitivity and capacity that you can track across visits.
Training is tailored to either hyposensitivity or hypersensitivity. For hyposensitive patients, you may work near the “desire to defecate” level, encouraging patients to label internal sensations and gradually lowering the volume with each inflation to help them detect earlier cues. For hypersensitive patients or those with urge incontinence, you may work closer to the strong-urge threshold, using repeated inflations while practicing urge suppression strategies such as diaphragmatic breathing, targeted pelvic floor contractions, and cognitive reframing to reduce fear of leakage.
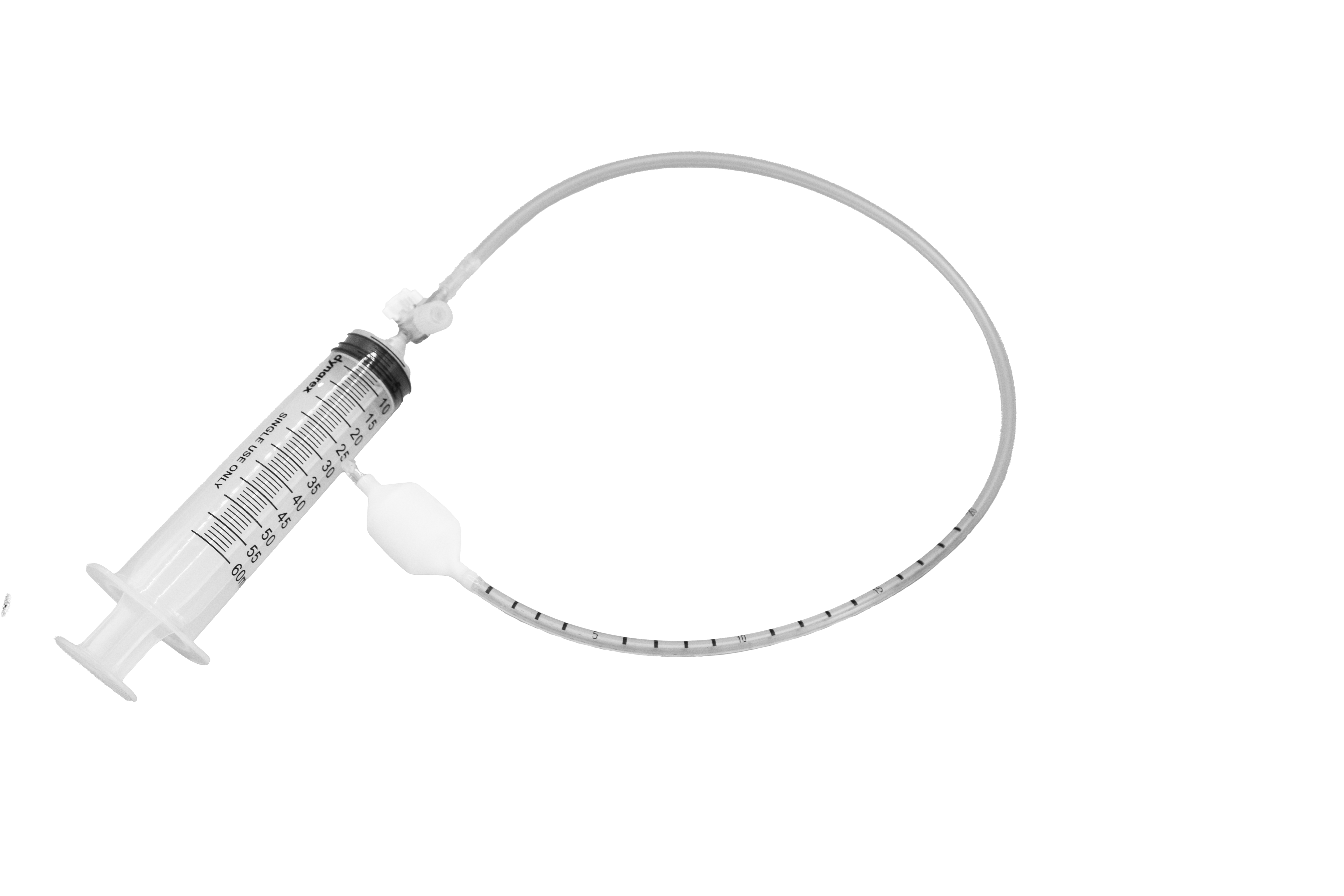
For these protocols, many pelvic floor physical therapists use a single-patient anorectal balloon catheter such as the SR1B anorectal expulsion balloon catheter or the SR2B anorectal expulsion balloon catheter for both air/water, which are designed for rectal sensory and expulsion training in pelvic rehab settings.
Balloon expulsion training for dyssynergia and outlet obstruction
For patients with dyssynergic defecation or outlet obstruction, the focus shifts to balloon expulsion. Whenever possible, position the patient on a commode or toilet simulator to approximate real toileting mechanics. Inflate the balloon to a volume that creates a clear “call to stool” sensation, and then coach the patient through a series of defecation attempts. Emphasize coordinated abdominal pressurization with simultaneous pelvic floor and anal relaxation, often using cues like allowing the belly to expand, leaning forward, and imagining the anus softening rather than “pushing through a closed door.”
If expulsion is difficult, you may apply gentle traction on the catheter during a coordinated effort to provide additional sensory feedback and motor learning. Over successive sessions, typical goals include reducing expulsion time, normalizing the pattern of pressure generation and relaxation, and decreasing the patient’s reliance on excessive straining or digital maneuvers.
Urge management and continence training
In patients whose primary complaint is urgency or fecal leakage, rectal balloon work can be used to rehearse “high-risk” scenarios in a safe, controlled way. With the patient sitting or standing, the balloon is inflated to a moderate urge level. You can then guide the patient through timed pelvic floor contractions, breathing techniques, and mental strategies intended to reduce urge intensity and delay defecation without panic. Over time, inflation volumes and hold durations are progressed to mimic real-life experiences, such as getting a sudden urge in a public setting.
This is also an ideal time to offer practical education, including how to interpret gas and stool cues, recognize “trustworthy” versus “untrustworthy” gas, and plan bathroom access in daily routines, framed in accessible, stigma-reducing language.
Combining rectal balloon training with PFMT and EMG biofeedback
Anorectal balloon work is most effective when integrated into a broader pelvic rehabilitation program that includes pelvic floor muscle training and, when available, EMG or manometry-based biofeedback. A common session structure is to begin with EMG or manometry in a comfortable position to establish baseline strength, relaxation, and coordination, then transition into balloon-based tasks that apply those skills to real toileting simulations.
Many research protocols use a series of supervised visits—often four to six sessions over several weeks—combined with a structured home program of pelvic floor exercises and toileting practice. In one trial of rectal balloon training as an adjunct to pelvic floor work in urinary incontinence, patients practiced multiple contraction–relax cycles daily over several weeks, using the balloon as a sensory cue and, in some cases, a low-level resistance. Similar principles can be adapted for constipation and fecal incontinence, with volumes, positions, and cues tailored to each patient’s impairments and goals.
Bringing anorectal balloon catheters into pelvic PT practice
For pelvic floor physical therapists, anorectal balloon catheters offer a way to deliver guideline-supported, highly specific interventions for patients whose bowel symptoms often persist despite general conservative management. By systematically assessing rectal sensation, practicing defecation mechanics, and rehearsing urge management, you can shift care from generic advice to measurable, skills-based rehabilitation. This approach aligns with emerging evidence and consensus recommendations while giving patients a clearer, more hopeful narrative about why they struggle and how targeted training can help.
Frequently asked questions
Which patients benefit most from anorectal balloon training?
Patients with dyssynergic defecation, outlet obstruction constipation, rectal hyposensitivity or hypersensitivity, chronic proctalgia, and fecal incontinence related to urge control issues are strong candidates for rectal balloon training.
Is rectal balloon training uncomfortable?
Most patients tolerate rectal balloon training well when volumes are progressed gradually and communication is clear. You can titrate inflation based on the patient’s feedback and stop at any point, which helps maintain comfort and trust.
How many sessions do patients usually need?
Research protocols commonly use four to six supervised biofeedback sessions over several weeks, plus a structured home program of pelvic floor exercises and toileting practice. In clinical practice, the total number of visits depends on symptom severity, comorbidities, and the patient’s ability to follow through with home strategies.